However, there are other times when pain flare-ups seem to come out of nowhere. Obviously, these are more difficult to handle. But with a little reflection, you might see that there were some events that lead up to the pain, as I did in my blog: How to Stop Freaking Out When You Hurt.
In either case, you can do several things to help yourself get through and past this difficult time. Starting with:
Step 1: Recognizing that flare-ups are a normal and expected part of the healing process. Like the graph at the top of the page shows, recovery from chronic pain doesn’t happen in a straight line. There are ups and downs, but there should be an overall upward trajectory.
 A flare-up might be seen as a set-back in your recovery. However, in his book, The Way Out, Alan Gordon, psychotherapist and executive director of the Pain Psychology Center in Los Angeles, put it well.
A flare-up might be seen as a set-back in your recovery. However, in his book, The Way Out, Alan Gordon, psychotherapist and executive director of the Pain Psychology Center in Los Angeles, put it well.
“Setbacks are like speed bumps on the road to a pain free life. They may slow you down but as long as you stay the course they can’t stop you.”
—Alan Gordon, LCSW
Fear is the fuel that intensifies a flare-up
Step 2: Understand the relationship between fear and pain. The more anxious and worried we are about the pain, the more pain we are likely to feel. In his book, Gordon talks about the pain-fear cycle, which is based on the Fear-Avoidance Model that I mentioned in my blog: Conquer Your Fear of Pain with Movement. If you look below, you will see my depiction of this cycle, with one additional factor added into the loop. At this point, though, I want to give Dr Howard Schubiner credit for this addition, which I learned in his course with Hal Greenham, BSc (Psych), Freedom from Chronic Pain.
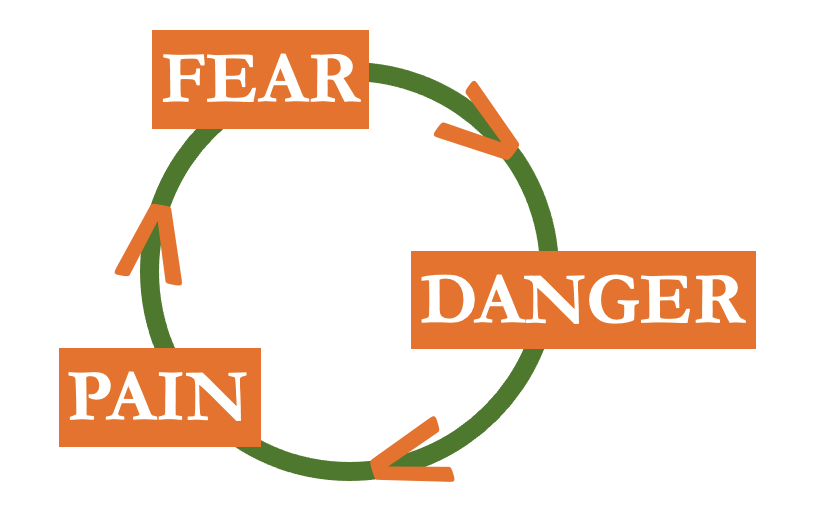 Now take another look at the cycle pictured to the right. Although this cycle, or a flare-up, generally starts with pain, I chose to put fear at the top of my image. Why, you ask? Because fear is the component of the cycle that keeps us going around and around the loop. It even accelerates how quickly we move around the circle.
Now take another look at the cycle pictured to the right. Although this cycle, or a flare-up, generally starts with pain, I chose to put fear at the top of my image. Why, you ask? Because fear is the component of the cycle that keeps us going around and around the loop. It even accelerates how quickly we move around the circle.
In order to understand how this works, let’s consider that you just felt the sensation of pain in your back, a site of previous injury. This is the start of your flare-up cycle. Your initial trip around the circle begins in the lower left quadrant with pain. When you experience pain, you first have an emotional reaction: fear. Then, this fear leads to the desire to figure out what is wrong and what to do or not do. Hence, we intensely focus on the pain. Gordon compares this intense focus to the vigilance of a hawk. The more we watch the pain, narrow in on the feeling and evaluate the quality of the pain, worry that we might be hurting ourselves and think negatively about the pain and our future, the more danger our nervous system senses. Danger, the next component of the cycle, is the signal that is communicated to the brain. (More on this in the next section.) This heightened attention on the pain makes us feel that the pain must be very dangerous. This, in turn, increases our pain and leads to more fear.
After our first trip around the circle, we are back at the top, stuck in fear. For our next trip around the loop and for all those that follow, fear is our starting point. Fear keeps us stuck in this escalating cycle of pain. Consequently, fear is also the point in the cycle where we can take action and break out of the incessant loop.
Pain and Your Brain
Pain plays an important role in our body: to protect us. Pain tries to keep us safe. Hence, when our brain receives more and more messages of danger, it raises our pain level to stop us from hurting ourselves. Note that the brain actually generates pain. The body merely sends the brain danger signals that the brain then interprets. And, one way that the brain reacts to these danger signals is to create pain. Read more about the brain’s role in generating pain in this blog: Your Brain Interprets Your Pain.
To explain this a bit more, let’s consider an example. When you break a bone, you don’t want to use that part of your body to protect it from further damage. In this case, the brain creates pain to keep your body safe. The brain doesn’t know the difference between an acute injury, such as a broken bone, and a flare-up of an old, chronic pain. All it knows is that the body is in danger. So, it responds accordingly. Therefore, as our perception of danger escalates, the brain becomes more and more concerned. It then responds by turning up the amount of pain we feel.
How to Reduce Your Fear
When your pain is intense, Gordon recommends self-soothing activities that make you feel good and calm your brain. He calls these avoidance behaviors. What makes you feel better when you are in pain? You might consider brainstorming a list now, before a flare-up happens, because when we’re in pain we don’t always think logically. Keep this list of calming activities handy so you can easily find it when needed. Here are some ideas to get you started:
- Use heat or ice
- Stretch and move
- Practice diaphragm breathing
- Get a massage
- Take a warm bath
- Lie down with your legs up
- Foam roll
- Light a scented candle
When you are having a pain flare-up, this is not the time to learn new techniques to reduce your fear (like mindfulness, journaling, body scan, mediation, etc.). It’s better to do this when you have less pain. Then, when you have recovered, consider choosing one new skill to learn that you can add to your list of calming activities in the future.
Increase your sense of safety
Step 3: Let your brain know you are safe. The physical sensation in your body, combined with your mental thoughts and strong emotions, create an internal environment of danger. Your body and brain feel under attack. This ramps up the pain. In addition to making yourself physically comfortable, as discussed above, you also need to take care of your brain. Consider what you tend to say to yourself during a flare-up.
- When is this going to end?
- How long is it going to last?
- I don’t have the time or energy for this!
- How bad is the pain going to get?
- What did I do this time?
- I can’t handle this! If this applies to you, read my blog: What Are You Afraid Of – Can You Handle It?
You probably have more to add to the list . . . Reading this inner dialogue, how do you think it affects your brain’s sense of safety? Not feeling warm and cozy, are you? Your words are raising more and more red flags, and the alarms are loudly ringing in your brain. To reverse this, first notice what you are saying to yourself. Then, secondly, send your brain safe messages. Try these:
- This too shall pass.
- Everything is going to be okay.
- I’m safe and strong.
- The pain is temporary.
Or a couple from leading pain educator Adriaan Louw, PT, PhD:
- Hurt does not equal harm.
- Sore but safe.
Flare-ups are unpleasant and unavoidable. How you mentally and emotionally respond affects your pain. Fear and danger exacerbate your pain, while feeling calm and safe reduces the pain. Next time you have a flare-up, if there is a next time (hopefully not), try the steps outlined here for a quick recovery. And if you follow these steps, please leave a comment to let me know how it went.



